For one in 20 men, the uncertainties of life are reflected in seeking a Vasectomy reversal.
Vasectomy Technique and Success Rates of Reversal
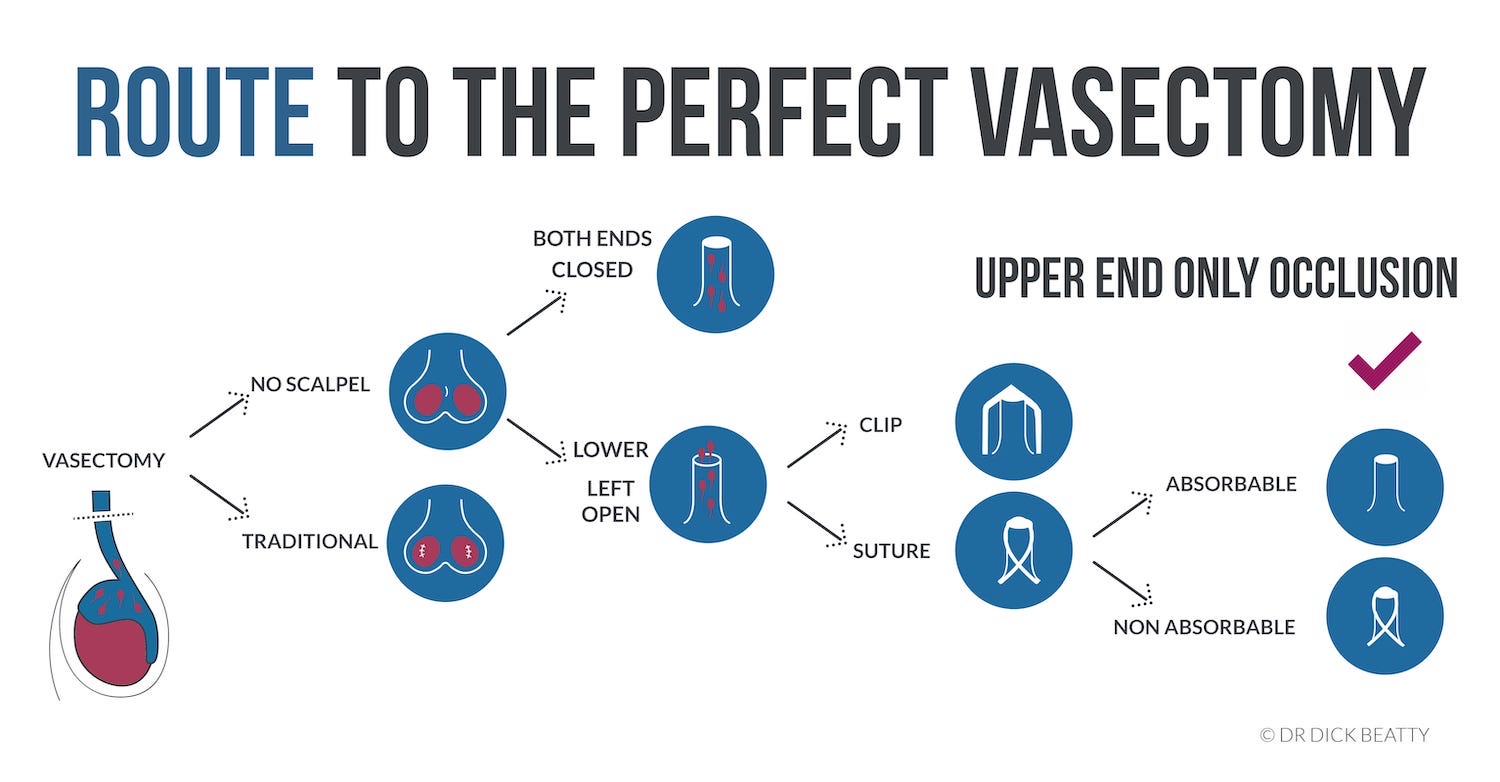
There is a tension between an effective vasectomy method and one that is easier to reverse. After all, the easiest vasectomy to reverse is one that did not work in the first place.
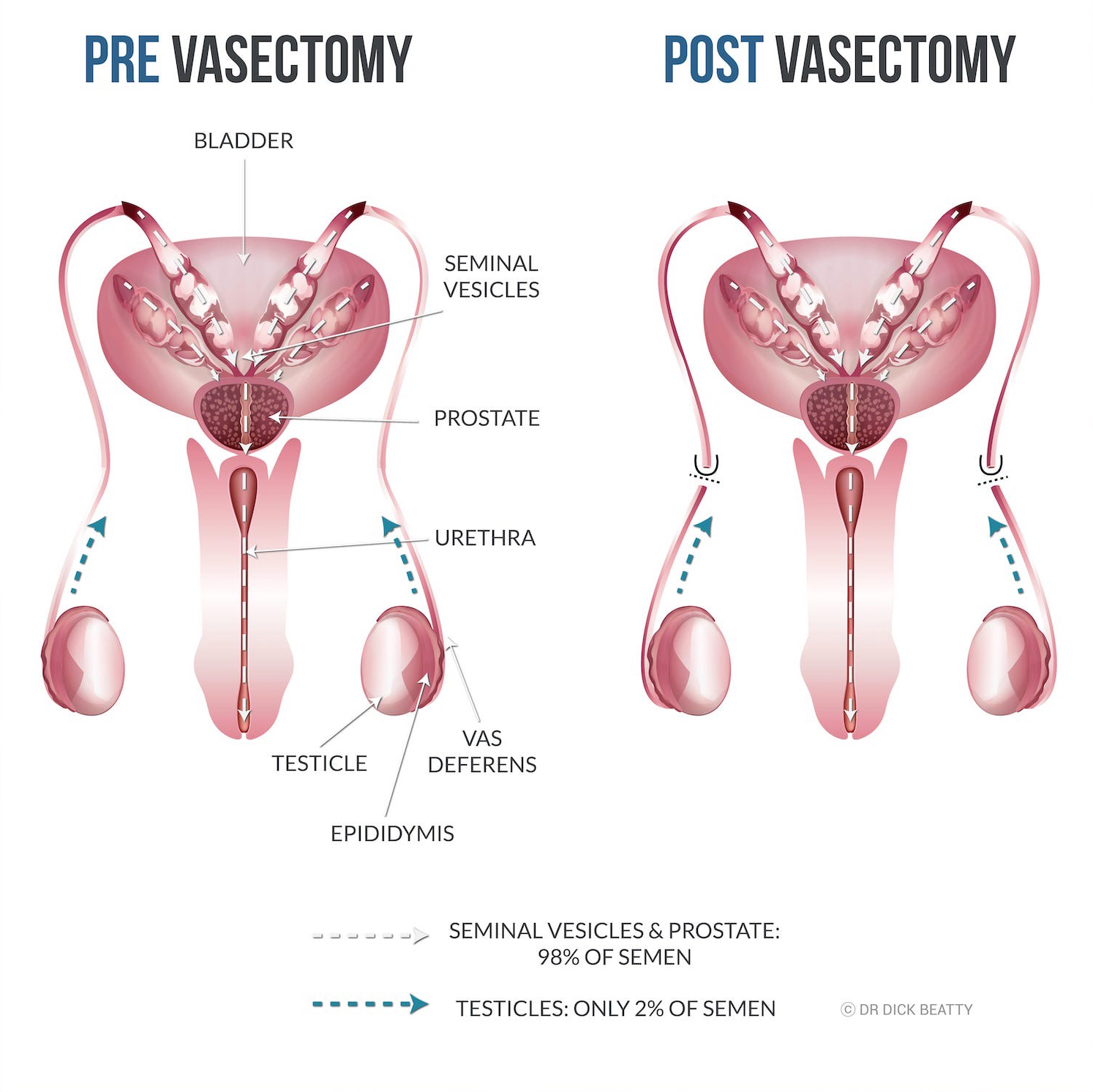
Vasectomy involves cauterizing the vas deferens and cutting it, while reversal reconnects the viable vas that has not been cauterized. In other words, the less cautery, the better for reversing – at least in theory.
Open-ended vasectomy may less challenging to reverse due to less cautery, in contrast to closed vasectomy, which often requires more cautery.
The closed method typically relies entirely upon cautery to block the vas deferens. Cauterizing a long segment (eg. >5cm) is required to keep the failure rate to a minimum (still around 1%).
In comparison, an ‘open-ended‘ vasectomy relies on separating the ends (fascial interposition using a clip or dissolvable stitch) to block the tube. Cautery is only used for the upper end. Additionally, during surgery, the doctor may expect to achieve perfect end separation, potentially eliminating the need for cautery (unproven).
It is important to remember that the primary goal of a vasectomy is to prevent the passage of sperm and not necessarily to optimize the chances of a successful reversal. However, for younger men or those who have not yet fathered children, the potential for a future reversal may be a consideration when deciding on the amount of cautery used.
Vasectomy Reversal versus IVF
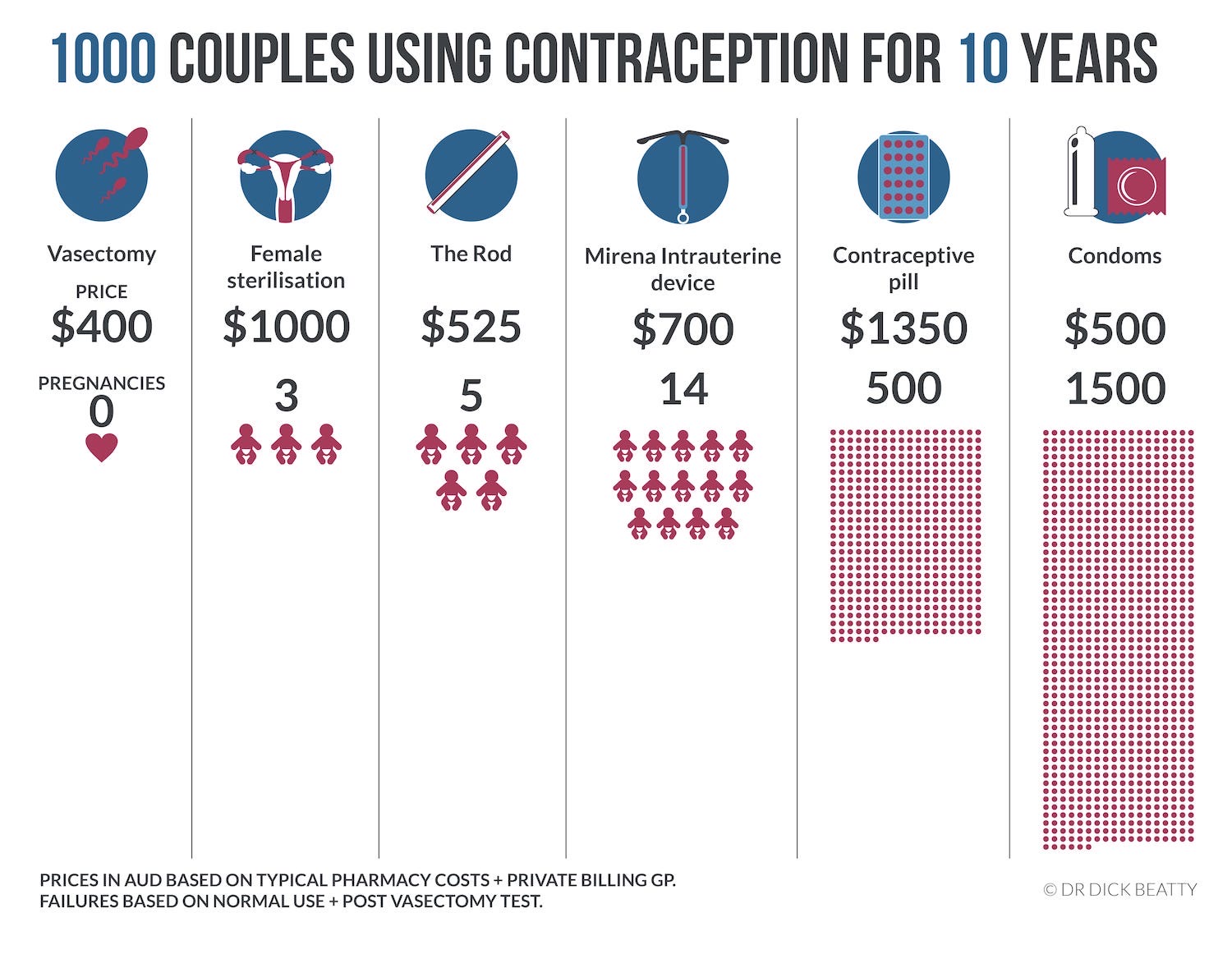
After a vasectomy, sperm can be extracted from the scrotum using a needle (via ICSI) for use in IVF. However the success rate of IVF is around 30%, but it may be much lower depending on fertility factors such as maternal age.
A peer-reviewed article states that Vasectomy Reversal, compared with IVF, ‘is typically more cost-effective and is the favoured approach for patients desiring multiple pregnancies with unimpaired female partner fertility.‘
Reversal success rates
A successful vasectomy reversal is indicated by the presence of a large number of motile (mobile) sperm, although this is not always guaranteed to result in a pregnancy.
The success rate ranges from 50% to over 90%, depending on various factors.
The interval between the vasectomy and a reversal is the most important factor. A large 1991 study is shows a gradual reduction in success as follows:
- < 3 years: motile sperm 97%, pregnancy 75%
- 3-8 years: motile sperm 88%, pregnancy 53%
- 9-14 years: motile sperm 79%, pregnancy 44%
- >15 years: motile sperm 71%, pregnancy 30%
Reversal Technique
There are two types of reversal operations: vasovasostomy, which re-connects the two ‘ends’ of each Vas Deferens, and Vasoepididymostomy, which connects the epididymis with the upper end.
Vasovastomy is the most common procedure, while Vasoepididymostomy is reserved for more complex cases. A vasoepididymostomy is a more demanding surgery because the Vas deferens is larger than the Epididymis. In other words, two tubes of different diameters are connected.
Vasectomy reversal requires microsurgery that is technically demanding – ‘The vas deferens (VD) has a luminal diameter of 0.3–0.5 mm … Performing microsurgery on such a delicate tissue is certainly challenging, and as with any procedure, outcomes improve with experience.’
Researching the success rate of vasectomy reversal in your area is ideal. According to a 2021 study of 107 reversal doctors in the USA, there is a significant lack of transparency in the publicly available information from vasectomy reversal practices.
How can you find out which Urologist to see? Search ‘vasoepididymostomy’ to pick up those urologists who can perform this surgery when standard reversal surgery (Vasovasostomy) will not work. Look at their website and get a feel for how many vasectomy reversals they do.
See your primary care doctor and get a referral to a Urologist who performs the surgery regularly.
Price of Vasectomy Reversal
The total price for a vasectomy reversal might be around $10,000 AUD, with a Medicare rebate of under $1,000. Private health cover can reduce out-of-pocket expenses by several thousand dollars.