No-Scalpel Vasectomy
and Open-Ended
Table of Contents
The Terminology
No-Scalpel Vasectomy
The Tubes
Upper End & Lower End
Each of the two tubes is divided, leaving two ends.
The upper end is the end nearest the groin, referred to as the abdominal end. The lower end is the end nearest the testicle, referred to as the testicular end.
The Fascia
Fascial Interposition
Open-Ended Vasectomy
Whiteboard Video
What is No-Scalpel Vasectomy?
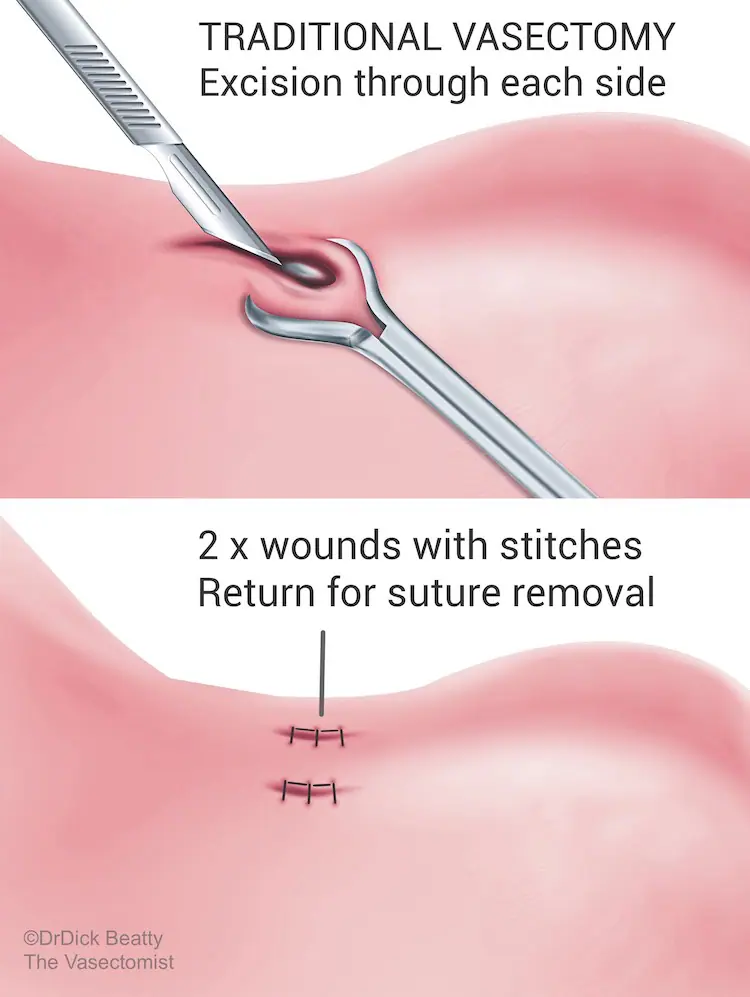
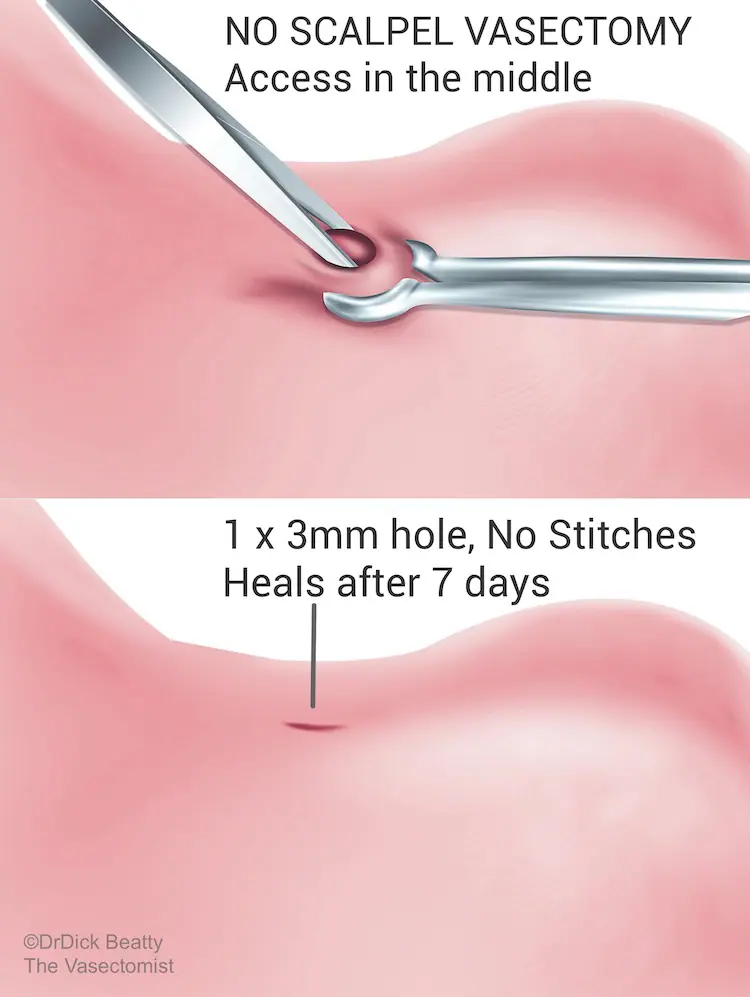
No-Scalpel Vasectomy (NSV) is is a type of ‘minimally invasive’ vasectomy – the vasectomy version of keyhole surgery. NSV leaves a small 2-3mm hole at the front of the scrotum. No stitches are required, so you don’t have to come back for stitch removal. Minimal trauma to the tissue means that you can return to work and physical activities sooner. On the other hand, traditional vasectomy requires incisions and stitches on both sides of the sac.
Do we really need guidelines to confirm that vasectomy should effectively be gentle? Maybe not, but it’s comforting to know that The UK Vasectomy guideline (FSRH 2014) states that ‘a minimally invasive approach should be used to expose and isolate the Vas Deferens during vasectomy as this approach results in fewer early complications in comparison to other methods.’
NSV is also recommended above traditional vasectomy in The American Urological Association Vasectomy Guideline which specifically states in their amended 2015 guideline that ‘Minimally Invasive Vasectomy should be used for Vas Isolation.’ The European Association of Urology Guidelines on Vasectomy guideline (2012) adds to the consensus.
No-Scalpel Vasectomy is a superior method of gaining access to The Vas Deferens. However, NSV is 20+-year-old technology. A crucial but surprisingly little-known fact is that No-Scalpel Vasectomy (NSV) simply describes the way of getting to the tubes – no more, and no less.
How are the tubes blocked?
Most Vasectomies these days are described as No-Scalpel Vasectomy, which is akin to saying keyhole surgery – but says nothing about how the tubes are blocked.
Most guys think that cutting the tubes is enough – an idea pervaded by the term ‘snip.’ You can’t simply cut the tubes because they will almost certainly grow back. Another common misunderstanding is that the tubes are tied, which they are not.
Let’s introduce the vasectomy buzzword that separates one vasectomy from another: Occlusion.
What really separates types of vasectomy is the method of occlusion and not how to get to them (NSV)
Different methods of occlusion are:
- Electrocautery to the internal lining of the tube (the lumen) – with a machine that looks a bit like a laser.
- Thermal cautery to the lumen (cautery using heat) – typically with a low-tech battery-operated pen device.
- Capping the end of the tube with its outside lining called fascia (fascial interposition).
- A combination of cautery and fascial interposition.
Open .v. Closed Vasectomy
You now understand that ‘no-scalpel vasectomy’ simply means the doctor has deftly got to the tubes. What next? Do you block the upper end, the lower end, or both? This is where things get a little convoluted (incidentally a bit like the lower end of the tubes).
Strangely enough, removing a segment of vas is not effective because the two ends will simply re-attach.
Dr Dick Beatty gets out the whiteboard with two scenarios:
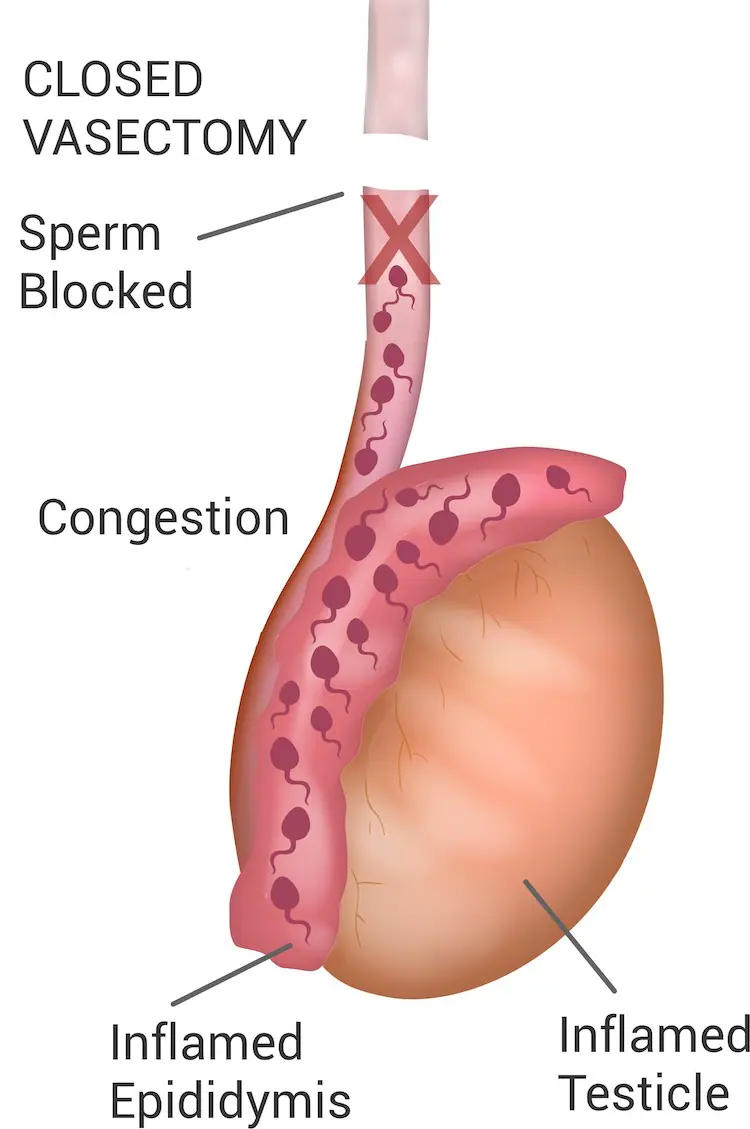
Both ends are occluded
Closed Vasectomy blocks the lower end, potentially causing ‘blue balls’ from an increase in backpressure. You can’t just cauterise one end and leave the other open, or the tubes have a 10% risk of growing back. Closed Vasectomy, therefore, requires both the upper and the lower end to be occluded – typically with electrocautery.
Dr Dick Beatty started out with this method.
The concern with closed Vasectomy is that the sperm have nowhere to go, which may lead to discomfort caused by congestion.
The rate of failure tends to be higher – and great care needs to be taken to avoid an unacceptable failure rate.
The lower end is left open.
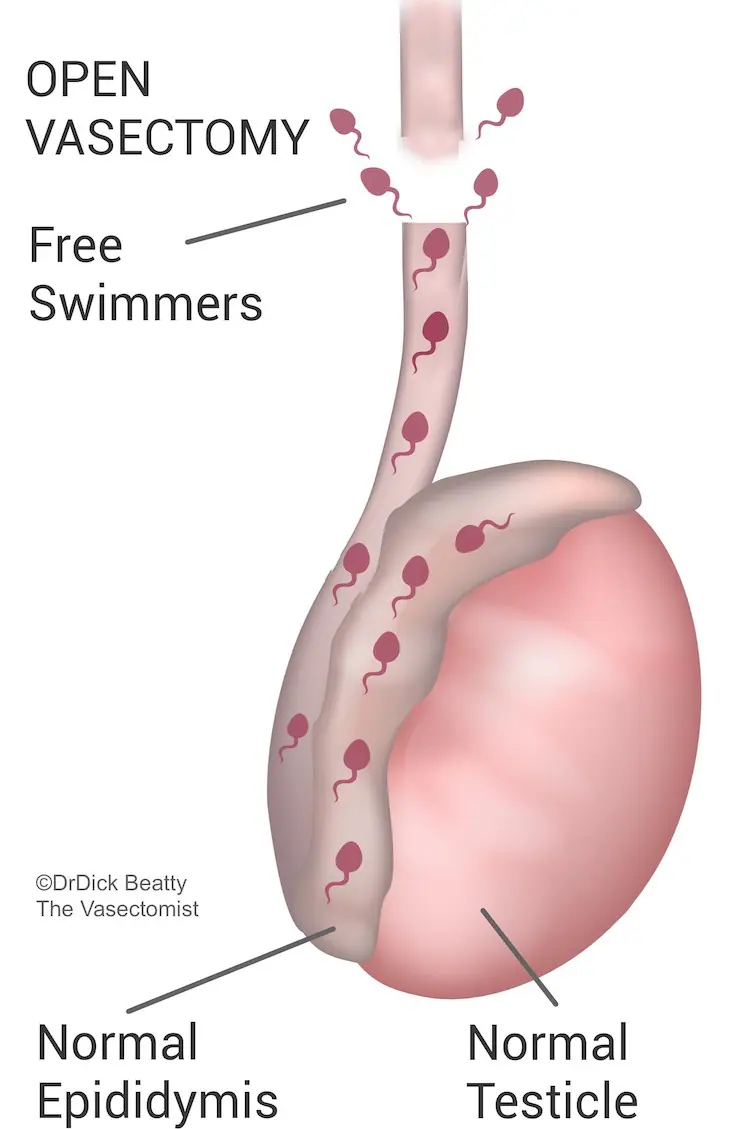
Open-Ended Vasectomy describes the scenario where only the upper end is occluded. In other words, The lower end is left alone so that sperm are free to swim upstream from the testicle through the open end.
Open-ended vasectomy is considered to be the gold standard method of occluding the vas deferens.
Fascial Interposition
Fascial Interposition (FI) is regarded by leading Vasectomists as the gold standard vasectomy technique. Why? Because FI is the technique that allows the vasectomy to be open-ended.
The vas deferens have a thin, slippery outer structure called fascia, likened to the outer layer of a sausage. The fascia is gently pulled over the ‘stump’ of the cut vas and secured in place with a titanium clip or suture (Dr Beatty uses absorbable suture). Unlike cautery, FI is such an effective method of occlusion that it only needs to be performed on one end.
FI to the upper end allows the lower end to be left alone or ‘open’; open-ended vasectomy may reduce post-procedure discomfort. The theory goes that sperm swim out of the lower tube after an Open-Ended Vasectomy. An experiment in rats demonstrated that the tubes that are left open do, in fact seal themselves closed within a few weeks of a vasectomy. However, closure would certainly be slower than the abrupt surgical closure of a closed vasectomy.
Research comparing open to closed vasectomy suggests that Open-Ended Vasectomy does indeed result in less post-vasectomy discomfort. However, research is not 100% conclusive, which explains why vasectomy guidelines do not (yet) categorically state that open-ended is better than closed vasectomy. Closed Vasectomy is typically performed in The UK, whilst Open-Ended Vasectomy is more likely to be performed in The US, Canada and Australia. Doctors are trained by vasectomists using the method they were trained in.
Furthermore, Open-Ended Vasectomy (AKA Fascial Interposition) improves the success rate of vasectomy while cautery to both the upper and lower ends is more likely to fail – particularly if the use of cautery is minimised. Aggressive cautery is more difficult to reverse and takes longer to heal than Open-Ended Vasectomy.
Vasectomists who have performed both open-ended and closed vasectomy will usually continue with Open-Ended method, attesting to extremely low failure rates (less than 1 in 1,000).
