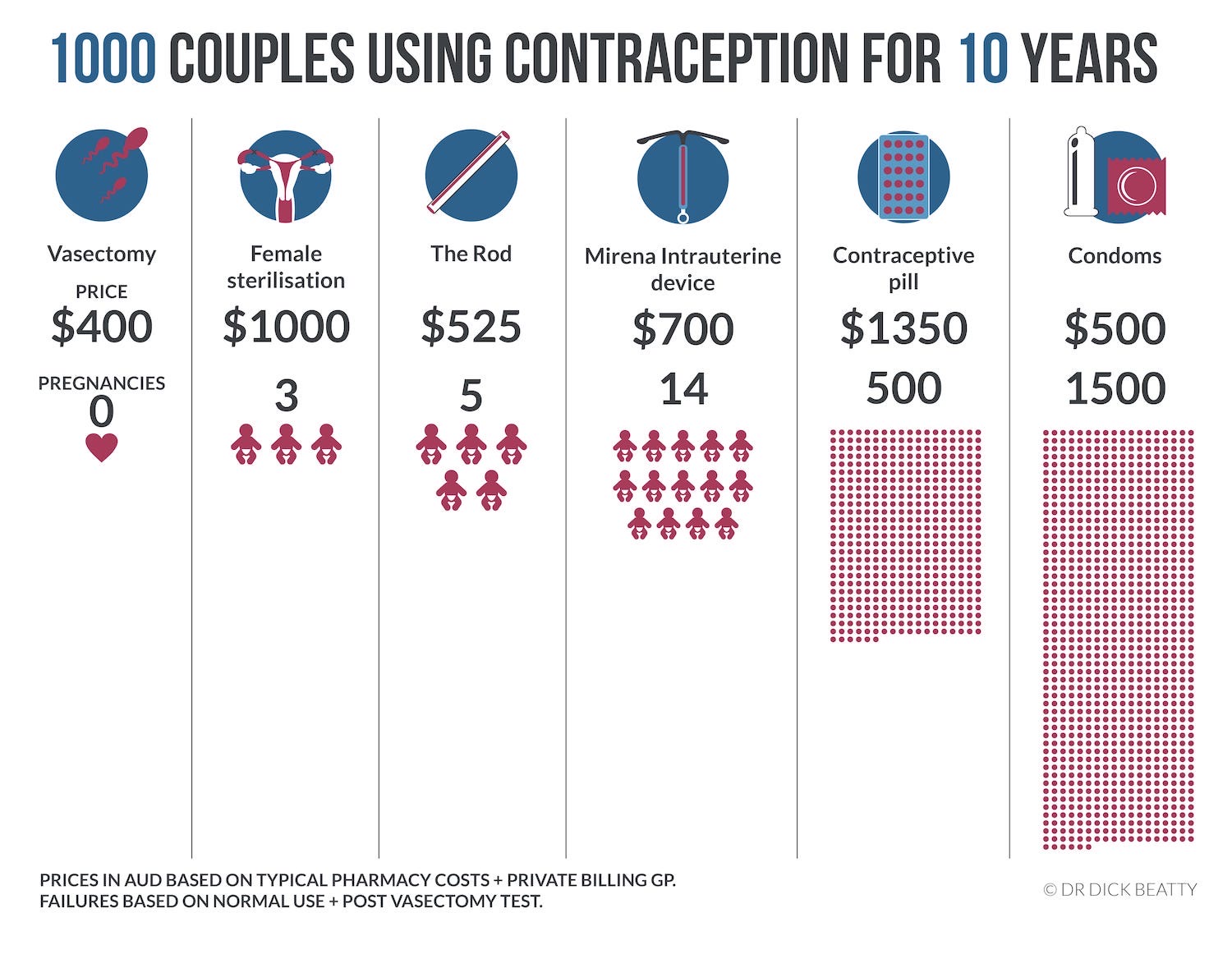
| Risk of Pregnancy PER YEAR | Main Benefits | Main Risks | Issues |
|---|
| Combined Pill | 7% per year (normal use) | Low Failure Rate, can reduce period bleeding, can have cycles back-to-back. Often Beneficial for conditions like acne or hirsutism. | Deep Vein Thrombosis & Cardiovascular Risk Factors to evaluate include Body mass index, Smoking, Migraine with aura, Family history, increasing age, high BP, Cholesterol, Diabetes, kidney disease etc. | Can forget to take the pill. |
|---|
| Progestogen Only Pill | 9% per year (normal use) | Used as a 2nd line oral contraceptive when the combined pill is not recommended. No increased cardiovascular or thrombotic risks. | Australian licensed mini pills need to be taken in a 3 hour window each day. | The minipill is unforgiving when forgotten – failure rates are high. |
|---|
| Progestogen Injection | 6% per year | No increased cardiovascular or thrombotic risks. Periods often disappear completely within 12 months. | Progestogenic side effects are usually manageable but women may sometimes report weight gain, mood or changes. Periods often erratic to start with. | 3 monthly visits to your doctor & practice nurse to get the injection. Need a pregnancy test if late for your next injection. |
|---|
| Progestogen Implant (rod) | 0.05% per year | Periods often disappear completely within 12 months. | Persistent bleeding beyond 6 months in around 15% of women may require the implant to be removed. | 3 yearly implant in the inner side of the left upper arm. |
|---|
| Intrauterine Device – Mirena | 0.2% per year | Periods usually disappear completely within 12 months – often good for heavy or painful periods. | Risk of uterine perforation is around 1 in 1000. Rarely infection or migration of the device. | 5 yearly re-insertion. Few GPs currently provide this service & most women need a referral to a gynaecologist. |
|---|
| Condom, Cap, Ring | Condom 18% Cap 12% | Caps, Diaphgragm & Vaginal Ring. | no systemic risks. Higher rate of failure than many other methods of contraception. | Suits only a few women and couples – comes down to personal preference & guidance on use from a health practitioner. |
|---|
| Female Sterilisation | 0.5% risk | Low failure rate at around 1 in 200 | Higher failure rate & risks (surgical + Anaesthetic) than The Snip. | Day Case in a hospital. |
|---|
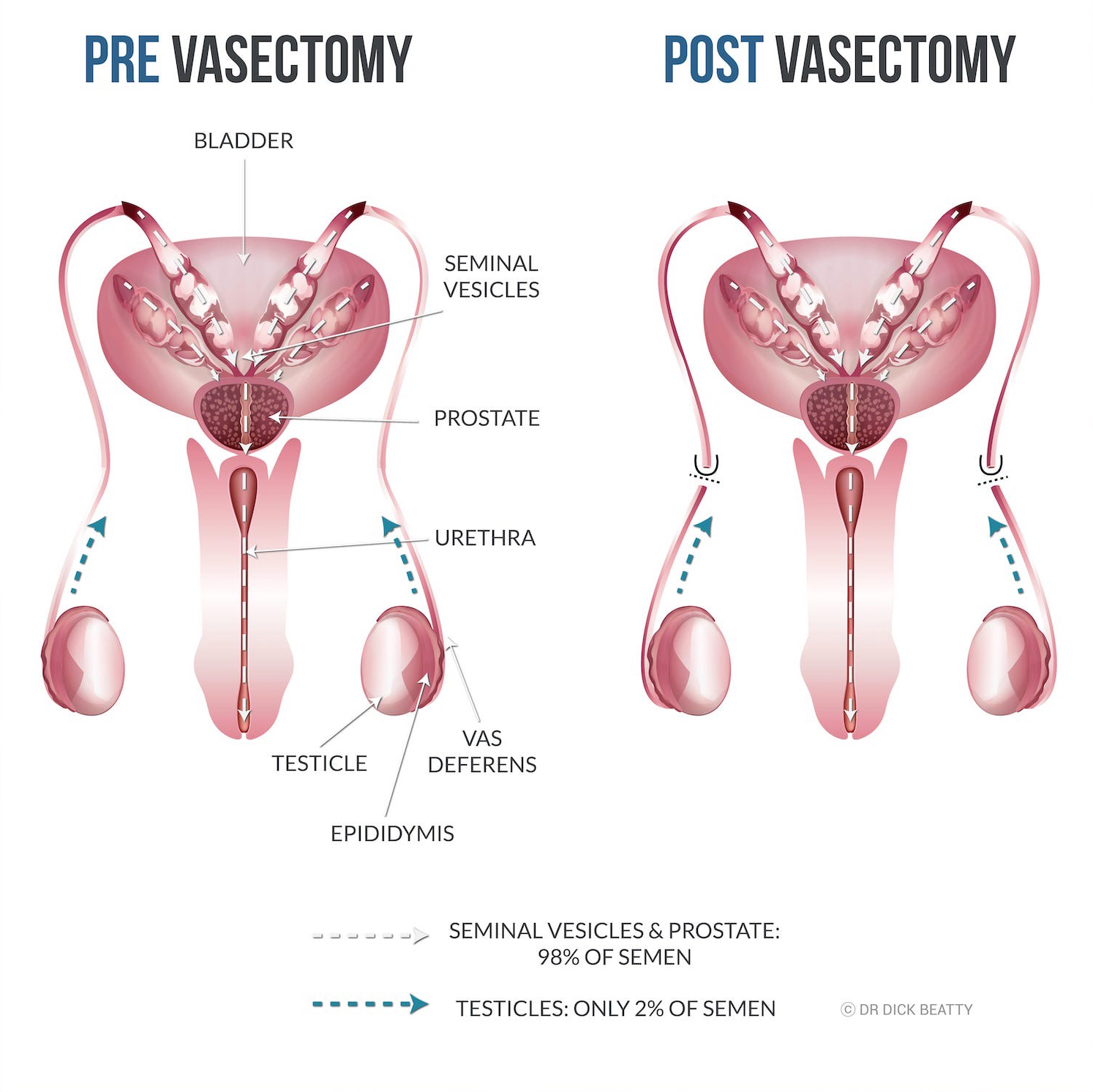
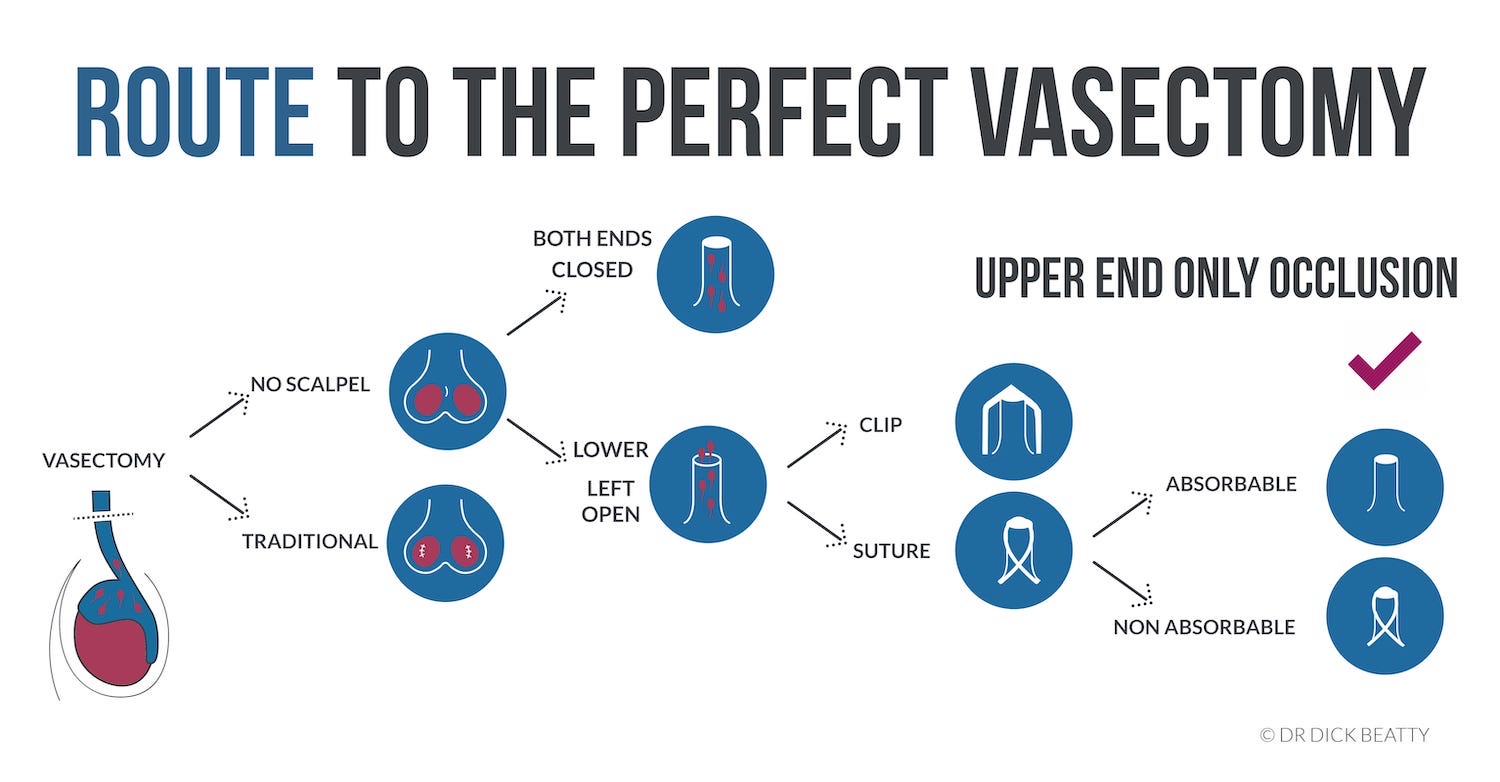
| Vasectomy | 1 in 3000 lifetime (after test) | The lowest failure rate. Men can get involved! | Post vasectomy discomfort affects around 1 in 50 guys. | The most important thing is to continue contraception until you get the all-clear after the semen analysis. |
|---|